In this post, I want to talk about a newer modification of radical prostatectomy that I have been practising for some time. As my patient results have come in – and as other centres have published theirs – it has become clear that this technique, known as Retzius‑sparing radical prostatectomy, is transforming early outcomes for continence and, potentially, potency. In many series, pad‑free continence rates shortly after surgery are 3 times higher than with the conventional approach.
Updated August 2017 with findings one year later: Retzius-sparing radical prostatectomy: one year on
What is Retzius‑sparing radical prostatectomy?
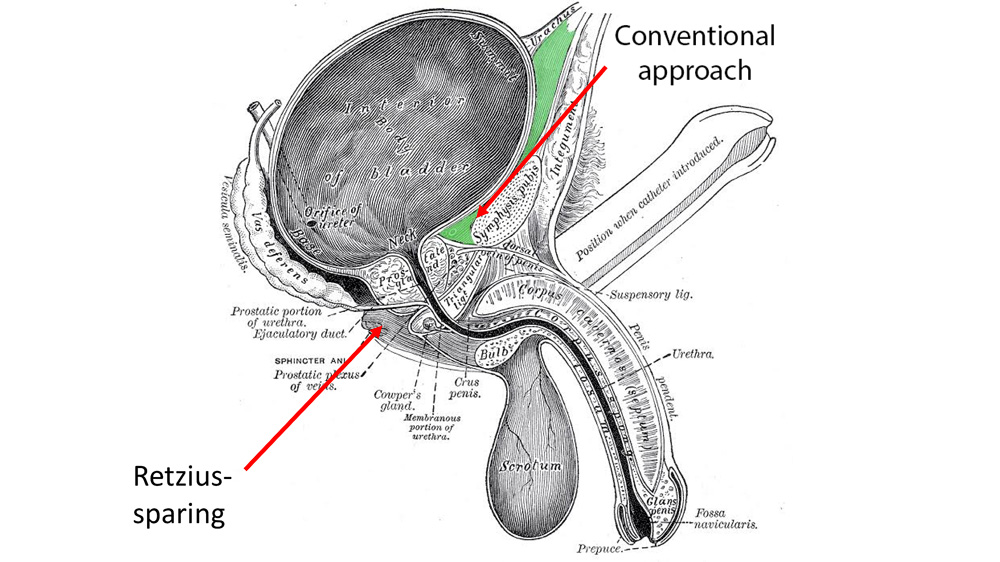
Retzius‑sparing prostatectomy is a way of removing the prostate that approaches it from behind the bladder (posterior approach) rather than through the space in front of it. The key idea is to avoid disturbing the “cave of Retzius” – the anatomical space between the pubic bone and the prostate that plays a major role in urinary continence and also carries arteries that help supply the penis.
Why the cave of Retzius matters
Anders Retzius (1796–1860) was a Swedish professor of anatomy who gave his name to this space. It is bounded by the pubic bone in front and the prostate behind. Its “floor” is formed by:
- Puboprostatic ligaments, short but very strong bands anchoring the prostate to the pubic bone, and,
- The endopelvic fascia, sheets of tough connective tissue that converge on the pelvic floor.
These structures help maintain continence. Important arteries to the penis also pass through the region. In short, how we approach the cave of Retzius during surgery is critical to a patient’s final outcome.
How the Retzius‑sparing technique differs from the conventional operation
In a conventional robot-assisted radical prostatectomy (often called RARP), the cave of Retzius is opened to reach the prostate: fat and connective tissue are removed, the puboprostatic ligaments are divided and some of the arterial inflow to the penis may be interrupted. All of this can contribute to post‑prostatectomy incontinence and erectile dysfunction.
By contrast, the Retzius‑sparing prostatectomy technique approaches the prostate from below the bladder. Because the positions of the bladder and prostate are “reversed” from the surgeon’s point of view, the anatomy looks different to the novice, but this rapidly becomes the new normal. I have now completed over 1,000 of these procedures. Even the anastomosis – re‑joining the bladder and urethra – is performed in reverse order compared with the conventional method, with the front wall completed first.
Retzius‑sparing prostatectomy steps (at a glance)
- Enter the posterior plane (behind the bladder) to expose the prostate without opening the cave of Retzius.
- Perform precise nerve‑sparing (no cautery on the neurovascular bundles in suitable cases).
- Preserve the puboprostatic ligaments, endopelvic fascia and dorsal venous complex where possible.
- Reconnect the bladder to the urethra with the front‑first anastomosis.
What do the published results for Retzius sparing prostatectomy show?
The largest early experiences came from Ospedale Niguarda in Milan (Professor Aldo Bocciardi) and Yonsei University Hospital in Seoul (Professor Koon Rha). In a series of around 200 cases each, both groups reported immediate continence (no pads) in ~92% of their patients.
Having spent a week with Professor Rha in Seoul in June 2016, I performed the UK’s first robotic Retzius‑sparing radical prostatectomy on 4 July 2016, and the UK’s first laparoscopic Retzius‑sparing radical prostatectomy three days later. In my first 20 Retzius‑sparing cases, the results mirrored the published data: at 4 weeks after surgery, 80% were pad‑free and 20% used one small safety liner per day (100% at 0–1 pads/day).
For comparison, in my last 100 conventional (non‑Retzius) cases – already considered excellent – only 12% were pad‑free and 10% used one small safety liner per day at 4 weeks (22% at 0–1 pads/day). Early potency data also looked better than with the standard approach.

Professor Christopher Eden & Professor Rha in Seoul
One year on (2016–2017): the UK experience we presented
We extended the technique to more challenging cases – larger prostates, larger patients, and men with previous pelvic or prostate surgery – and by mid‑2017 had used it in over 120 men. We presented the first 40 UK cases at the British Association of Urological Surgeons (BAUS) Annual Scientific Meeting in Glasgow on 28 June 2017, and our talk was selected for the meeting highlights. Read the full article here.
Here are the key findings compared with non‑Retzius procedures:
- Operating time: on average 23 minutes shorter.
- Complications: lower overall (2.5% vs 8.0%).
- Catheter: most patients had a suprapubic rather than urethral catheter (often more comfortable).
- Catheter duration: removed 6 days earlier.
- Cancer control: similar in both localised (T2) and locally‑advanced (T3) disease.
- Continence at 4 weeks: 0 pads/day in 90%, 0–1 pads/day in 97.5%.
- By 12 weeks: 100% pad‑free in this series (40 patients), versus 66% at 12 weeks in my conventional series. My 12‑month pad‑free rate following conventional surgery was already 97.4%, regarded as world‑class, but the Retzius‑sparing approach delivered continence earlier and at a higher rate.
These findings were later published as “Urinary continence four weeks following Retzius‑sparing robotic radical prostatectomy: The UK experience” in the Journal of Clinical Urology. A video of the technique is also available.
What might explain the continence advantage?
Preserving the components of the cave of Retzius – the puboprostatic ligaments and the endopelvic fascia – appears to preserve the structural support of the external urinary sphincter, which translates into its better function and earlier pad‑free recovery.
What about potency?
There is a strong anatomical rationale for improved erectile function: by avoiding the cave of Retzius, we can better preserve arterial inflow and the neurovascular bundles that run close to the prostate. Longer follow‑up is needed to separate the effect of technique from patient selection, but our early observations suggested potency may recover more quickly when nerves can be spared and cautery is minimised, though larger series and longer follow-up are needed to confirm this.
Our surgical platform and philosophy
At Santis Health, we exclusively perform robotically‑assisted prostate surgery using the da Vinci Single Port (SP) Robot, which allows prostate removal through a single 4 cm incision. Our focus is on nerve‑sparing, meticulous haemostasis and gentle tissue handling – all of which align naturally with the Retzius‑sparing philosophy.
If you’re gathering information about treatment, you may also find these pages useful:
- Robotic Radical Prostatectomy – how we perform prostate removal and what to expect.
- Private Prostate Cancer Screening & Diagnosis – PSA testing, MRI and biopsy pathways.
Who might benefit from a Retzius‑sparing consultation?
- Men who prioritise early return of continence after surgery.
- Men considering surgery for localised or locally‑advanced prostate cancer.
- Men with larger prostates or a history of previous pelvic or prostate surgery.
- Those interested in exploring nerve‑sparing options to maximise erectile function recovery.
How Santis Health can help
Ready to explore your options? Book a consultation to speak directly with one of our prostate cancer surgeons. In a focused session, we will review your MRI/mpMRI, biopsy report and PSA trend; confirm stage and risk category; assess your suitability for Retzius‑sparing and how much nerve‑sparing we can safely aim for; explain your expected timelines for continence and erection recovery; and agree on a personalised plan.
If Retzius‑sparing isn’t the best option for you, we’ll explain why and recommend the safest, most effective alternative – so you can decide with confidence.

